Formation and Maturation of Phagosomes in Infected Mammalian Cells
The Basics
When a microorganism enters the sterile section of the human body, it is usually readily identified by specialized immune cells (phagocytic cells) which take up, kill, and destroy the invader. Some of these immune cells also present microbial antigens to other immune cells, informing them about the presence and the biochemical composition of the current enemy. In this way, the immune system can both mount an immediate response to the invader and maintain a "memory" about all the microorganisms it has encountered in the past to be ready for a possible new attack (‘innate’ vs. ‘acquired’ immune defence).
To ingest a microorganism, macrophages wrap it in a portion of their plasma membrane. This creates a new intracellular organelle, the "phagosome", which consists of the microorganism, its immediate surrounding space, and some former host cell membrane. Over the course of about an hour, this phagosome acidifies, is flushed with reactive oxygen intermediates, and fuses with pre-existing lysosomes to form so-called phagolysosomes. There, those microbes that are still alive are killed and most of the digestive work is done there. Again, this is how the defence normally works.
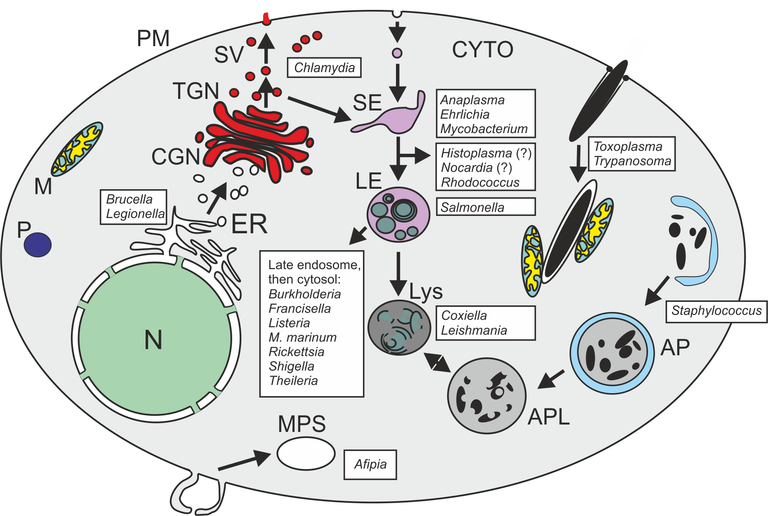
However: Some "intracellular", illness-causing microbes have found ways to reprogramme the macrophage not to kill them within a phagolysosome. Bacteria can employ any of the following three strategies for this purpose (see also Fig. below):
(1) The microorganism produces a factor which destroys the phagosome membrane. The bacterium thus released from the phagosome then multiplies in the macrophage cytoplasm (e.g., Listeria monocytogenes and Shigella flexneri);
(2) The microorganism changes the development of the phagosome compartment, and resides in a membrane-surrounded space which is not a phagolysosome (e.g., Mycobacterium tuberculosis and Legionella pneumophila);
(3) The microorganism has adapted to survive in the harsh environment of the phagolysosome and actually needs its otherwise lethal conditions (e.g., Coxiella burnetti and Leishmania mexicana).
We are particularly interested in the second group of microbes, i.e., those that leave a phagosome intact, but do not end up in a phagolysosome